Crucial Steps in Centralized Hospital Supply Management
Share
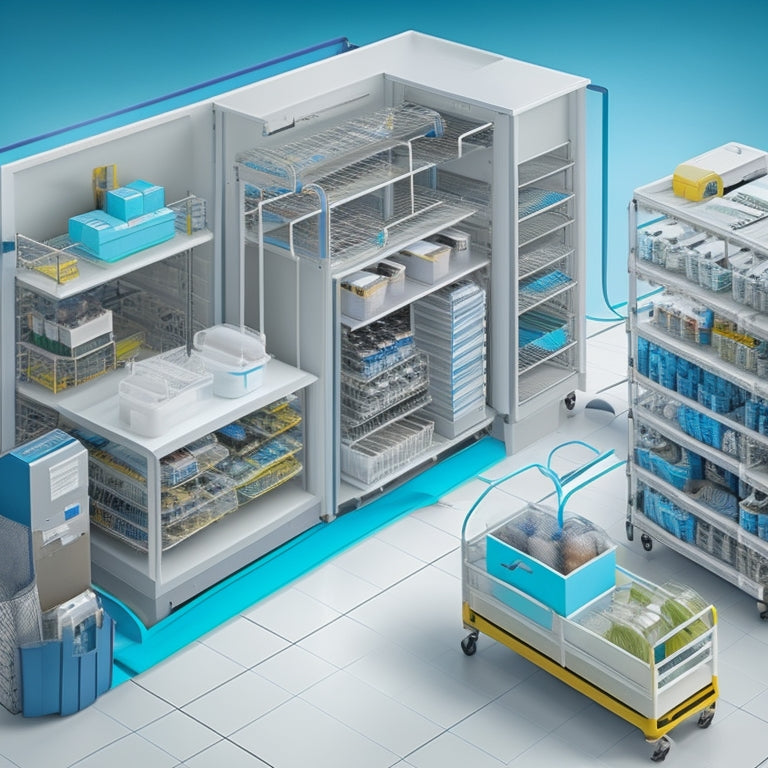
Effective centralized hospital supply management hinges on a cohesive system that incorporates key components. Central Service operations prioritize equipment maintenance and staff training, while the decontamination and sterilization process removes contaminants and microorganisms from supplies. Air flow control and safety measures prevent the spread of microorganisms, and sterile storage and inventory management guarantee the availability of sterile items for patient care. Additionally, strict temperature and humidity regulations are essential for the effectiveness of the sterilization process. By integrating these critical steps, hospitals can maintain a reliable and efficient supply management system that supports high-quality patient care and explores the intricacies of these processes.
Key Takeaways
• Implement One Way Work Flow for efficient supply handling and workflow efficiency in the Central Service department.
• Prioritize equipment maintenance to ensure proper functioning of sterilization equipment.
• Conduct regular inventory audits and optimize storage for accessibility and error reduction in sterile storage.
• Monitor and control temperature and humidity levels to ensure effective sterilization of hospital supplies.
• Emphasize staff training for efficient supply handling and proper sterilization techniques to prevent nosocomial infections.
Central Service Operations Overview
Every hospital relies on a centralized hospital supply management system, which is facilitated by Central Service, a department responsible for the centralized distribution of supplies to all hospital customers.
To guarantee seamless operations, Central Service prioritizes equipment maintenance, ensuring that all machinery is functioning at its best. Staff training is also essential, as it enables personnel to handle supplies efficiently and effectively.
Workflow efficiency is achieved through a well-organized One Way Work Flow, which prevents cross-contamination. Quality control measures are implemented to guarantee that supplies meet the highest standards.
Decontamination and Sterilization Process
Central Service's dedication to quality control measures extends to the Decontamination and Sterilization Process, an essential step in the Central Service One Way Work Flow that guarantees the removal of contaminants and microorganisms from hospital supplies. This process is vital in preventing nosocomial infections and ensuring the safety of patients and healthcare workers.
The Decontamination process involves physically or chemically rendering contaminated instruments safe to handle, following Standard Precautions that treat everything as infected or contaminated.
Here are key aspects of the Decontamination and Sterilization Process:
-
Textile packaging materials must be held at specific temperature and humidity prior to sterilization.
-
Sterilization techniques include steam sterilization, ensuring that all microorganisms are eliminated.
-
Proper sterilization prevents the formation of wet packs, indicating inadequate sterilization.
Air Flow Control and Safety
Effective air flow control is crucial in the Central Service department, as it prevents the spread of microorganisms and maintains a safe environment for hospital staff and patients.
To achieve this, a negative air flow system is implemented, drawing air into the room from surrounding areas. This prevents contaminated air from escaping and spreading infections.
Additionally, superheating precautions are taken to prevent steam temperatures from exceeding that of saturated steam at the same pressure, which can compromise sterilization processes.
Sterile Storage and Inventory Management
Proper sterile storage and inventory management are essential components of the Central Service One Way Work Flow, as they guarantee that sterilized items remain safe and ready for use in patient care. Effective sterile storage guarantees that items remain sterile until use, preventing contamination and nosocomial infections.
To achieve this, hospitals can implement the following measures:
-
Inventory tracking: Accurate tracking of sterilized items enables hospitals to monitor stock levels, reduce waste, and optimize storage space.
-
Storage optimization: Designating specific storage areas for sterilized items and organizing them by frequency of use can improve accessibility and reduce handling errors.
-
Regular inventory audits: Conducting regular audits helps identify and address inventory discrepancies, ensuring that only sterile items are stored and issued for patient care.
Temperature and Humidity Regulations
Maintaining ideal temperature and humidity levels is vital in the sterilization process, as it directly impacts the effectiveness of sterilization and the quality of sterilized items. Temperature and humidity control is critical for equipment sterilization, as it prevents superheating and ensures proper sterilization.
Textile packaging materials, used in linen packaging, require specific room temperature and humidity levels before sterilization to prevent wet packs. Strict adherence to packaging requirements is necessary to guarantee the quality of sterilized items. Failure to maintain ideal temperature and humidity levels can lead to inadequate sterilization, compromising patient safety.
Hence, it is essential to monitor and control temperature and humidity levels to ensure effective equipment sterilization and maintain the quality of sterilized items.
Frequently Asked Questions
What Measures Prevent Nosocomial Infections in Hospital Supply Management?
Implementing robust sterilization protocols and conducting rigorous infection surveillance are essential measures to prevent nosocomial infections in hospital supply management, ensuring a safe environment for patients and healthcare workers.
How Often Should Job Descriptions Be Reviewed and Updated?
'Like a well-oiled machine, job descriptions must be regularly tuned to guarantee Role Clarity, bridging Skill Gaps, and promoting a culture of safety; review and update them every 6-12 months to reflect evolving responsibilities and industry standards.'
Can Sterilized Items Be Stored in Non-Sterile Areas Temporarily?
Temporary storage of sterilized items in non-sterile areas poses significant Storage risks, compromising the efficacy of Sterilization protocols and increasing the potential for contamination, which can lead to nosocomial infections and patient harm.
Are All Hospital-Acquired Infections Considered Nosocomial Infections?
All hospital-acquired infections are considered nosocomial infections, as they occur within healthcare facilities, contributing to increased infection rates and disease transmission, underscoring the critical need for stringent infection control measures to safeguard patient safety.
What Happens if Linen Packaging Materials Exceed Weight Limitations?
In the delicate dance of supply management, exceeding weight limitations for linen packaging materials is like a misplaced step, compromising sterility and safety. It necessitates exploration of packaging alternatives, ensuring adherence to weight restrictions to prevent contamination and maintain the integrity of hospital supplies.
Related Posts
-

Revolutionize Your Kitchen With Clever Organizers
I've streamlined my kitchen by incorporating clever organizers that have transformed the way I cook and live. By maxi...
-

Discover Luxurious Self-Care Essentials at Foundry Home
At Foundry Home, discover a curated world of luxurious self-care essentials, expertly designed to elevate relaxation ...
-

Boost Kitchen Cabinet Storage With Lid Racks
You're looking to boost your kitchen cabinet storage with lid racks. By incorporating lid racks, you'll free up valua...


